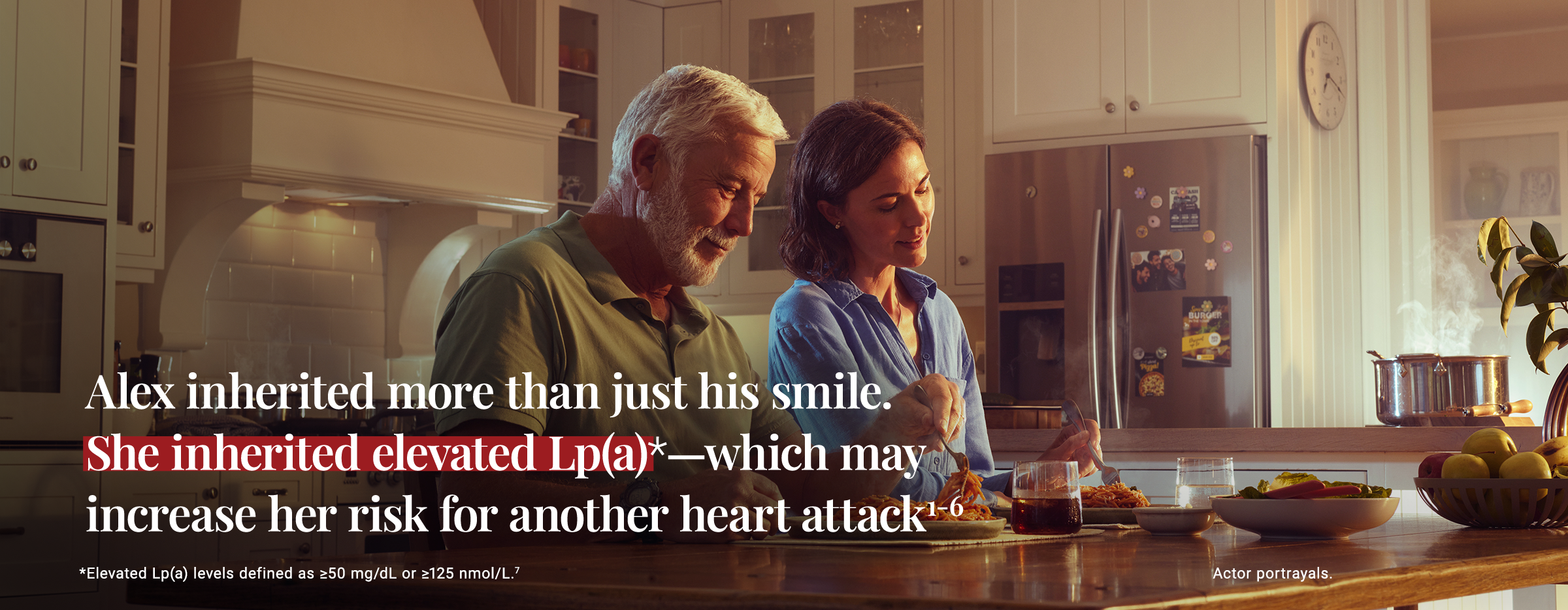
Elevated Lp(a) is a unique and genetically determined condition that can increase risk for ASCVD—in patients younger than you might expect1,2,8-11
Watch the video to see how Lp(a) testing can uncover a potential CV risk in patients with premature ASCVD (age <55 years in men, age <65 years in women)—and their family members.7,9
Despite its clinical significance, Lp(a) levels are often not measured as part of a standard CV risk assessment7,12,13
†Clinical relevance is unknown.
‡Atherogenicity was defined as the difference in coronary heart disease (CHD) risk per unit difference in Lp(a) or LDL particle number (molar concentration). This study was based on the UK Biobank population (>502,000 UK residents) who were predominately of European ancestry. The generalizability of the findings was tested in a replication cohort: the CARDIoGRAMplusC4D (Coronary ARtery DIsease Genome wide Replication and Meta-analysis [CARDIoGRAM] plus The Coronary Artery Disease Genetics) data set. Study did not differentiate between subjects with or without CHD at baseline. Analysis focused on the ApoB component of Lp(a).15
Lp(a) levels are ~90% genetically determined, typically established by 5 years of age, relatively consistent over time, and generally not affected by diet or lifestyle1,2,9,16
In one study, the higher a person's Lp(a) level, the higher their risk for a lifetime CV event16
The CV risk from elevated Lp(a) is independent of other risk factors2,5,7,17
Uncovering elevated Lp(a) can provide a deeper understanding of cardiovascular risk for your patients with premature ASCVD—and for their family members7,9
A surprising portion of patients with premature ASCVD may have elevated Lp(a)18
Professional organizations are recognizing the emerging importance of Lp(a) testing to inform next steps—including for your patients with premature ASCVD7,9,19-21
An elevated Lp(a) test result is actionable today by helping you better manage your patients' overall CV risk7
ASCVD, atherosclerotic cardiovascular disease; CV, cardiovascular; CVD, cardiovascular disease; LDL, low-density lipoprotein; Lp(a), Lipoprotein (a).
AHA/ACC/AACVPR/AAPA/ABC/ACPM
/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol. Circulation. 2019;139(25):e1082-e1143. 21. Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease. Circulation. 2019;140(11):e596-e646.